Skull base tumours are relatively rare, accounting for less than 5% of all brain tumours. A skull base tumour grows at the base of the skull. The skull base refers to the base or floor of the cranium, which is part of the skull on which the brain rests.
Skull base tumours can be benign or cancerous and are often difficult to diagnose and treat due to their location. They can grow from different types of tissues, including bone, cartilage, and nerves, and can cause a range of symptoms depending on their size and location.
There are several different types of tumours arising from or near to the skull base, including:
- acoustic neuromas
- adenoid cystic carcinoma
- chordomas
- chondrosarcomas
- craniopharyngiomas
- meningiomas
- paranasal sinus cancers
- pituitary adenomas
- Rathke’s cleft cysts
- schwannomas
Each of these arises from a different type of tissue and has its own characteristic features.
Skull base tumours can affect people of all ages and genders, but certain demographic groups may be more susceptible. For example, meningiomas are more common in women than men and tend to occur in people over the age of 40. Chordomas, on the other hand, are more common in men and tend to occur in people in their 30s and 40s.
Skull base tumours can be particularly challenging to treat due to their location and because they are close to critical structures such as the brainstem, cranial nerves, major blood vessels, the spinal cord and optic nerves that, if damaged, can have a life-changing impact on the patient. This can make traditional approaches to cancer treatment, such as surgery, difficult.
How are skull base cancers treated?
Treatment for skull base tumours depends on several factors, including the size and location of the tumour, as well as the type of tumour and the overall health of the patient.
In many cases, surgery is the primary treatment, but radiation therapy, including proton beam therapy, and systemic therapy, such as chemotherapy, may also be used.

Because of the complex nature of these tumours, treatment often requires a multidisciplinary team approach involving a range of specialists, such as neurosurgeons, clinical oncologists, and medical oncologists.
Proton beam therapy for Skull base cancer
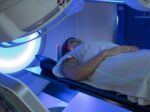
Proton beam therapy (PBT) is a type of radiation therapy that uses high-energy protons to target and destroy cancer cells. Unlike conventional radiotherapy, which uses X-rays (photons) or other types of high-energy radiation, it uses positively charged particles called protons.
During PBT, a machine called a synchrotron or cyclotron accelerates protons to high speeds and directs them into the body at the site of the tumour. The protons release their energy within the tumour, damaging the DNA of the cancer cells and causing them to die.
To learn more about what proton beam therapy is, read our information blog all about it here.
What are the benefits of proton radiation therapy in the treatment of skull base tumours?
There are several potential benefits to treating skull base tumours with proton beam therapy.
One advantage of intensity-modulated proton therapy over intensity-modulated radiotherapy with photons is that it can deliver a highly focused dose of radiation to the tumour while minimising the dose to surrounding healthy tissue.
This is because protons have a unique physical property called the ‘Bragg peak’, which allows them to deposit most of their energy within the tumour while sparing the surrounding normal tissue and avoiding ‘exit radiation doses’, which is inevitable when delivering traditional radiotherapy.
The greater precision that can be achieved with PBT compared with photon therapy potentially reduces side effects (acute toxicities) during and after radiation treatment (late toxicities), as it avoids exposing surrounding healthy tissue to unnecessary radiation, particularly beyond the tumour – called an exit dose.
This lowers the risk of treatment-related side effects that can result when healthy tissue is exposed to radiation. This is especially important for skull base tumours, where minimizing damage to surrounding structures is critical to preserving neurological function.
PBT gives physicians the option to deliver optimised radiation dose distribution directly to the source of the tumour in the skull. Because the risk of damaging surrounding tissues is greatly decreased, the radiation dose can also be increased for maximum effect.
Adjuvant radiation therapy refers to additional cancer treatment given after the primary treatment, such as surgery or chemotherapy, to reduce the risk of cancer coming back or to kill any remaining cancer cells. For example, a patient with a skull base tumour may undergo surgery to remove as much cancer as possible, followed by PBT to target any remaining cancer cells.

The emerging role of proton beam radiation therapy for chordoma and chondrosarcoma of the skull base
Proton beam therapy is a rapidly evolving technology for treating skull base tumours, and its effectiveness for this purpose is still being studied. However, while rare, skull-base chordomas or chondrosarcomas are some of the most difficult cancers to treat, and recent studies have found that pencil beam PBT is a promising treatment for tumours of this type.
Overall, research shows that PBT is effective and safe for these malignancies and that it should be considered an optimal treatment for limiting radiation dose to nearby organs at risk and delivering clinically effective doses to the tumour.
This study, for example, published in the International Journal of Radiation OncologyBiologyPhysics in 2009, reported a 5-year local control rate of 78% and a 5-year overall survival rate of 89% for 20 skull base chordoma patients treated with PBT.
Am I suitable for proton beam therapy?
Not all patients with skull base tumours are candidates for PBT, and treatment decisions are based on a thorough evaluation of each patient’s individual case.
A multidisciplinary team of specialists, including radiation oncologists, medical oncologists, and neurosurgeons, will help determine the best course of treatment for each patient. They will consider factors such as tumour type, size, location, and a patient’s overall health.

How long does proton therapy for skull base cancer take, and will I need to stay away from home?
A course of PBT is usually delivered over five consecutive days, usually Monday to Friday, followed by a two-day break. This can be repeated for up to 8 weeks, depending on the total dose of PBT that is prescribed. Each session is likely to take just 30 to 45 minutes.
Patients that live within travelling distance may choose to travel to the centre daily for treatment. But for patients who don’t live nearby or have come from abroad, this can present logistical challenges. Most PBT centres can advise or help patients and their families arrange travel and suitable accommodation while they are being treated.
At Proton International London we offer families a variety of places to stay within easy travelling distance and we ensure our patients’ time away from home is as pleasant as possible.
Where can I have proton beam therapy for skull base cancer in the UK?
There is a mix of both private and NHS-funded proton therapy treatment available in the UK:
NHS patients can be treated at The Christie Hospital in Manchester and at University College Hospital London (UCLH).
In conjunction with our first-class clinical colleagues at UCLH and UCLH Private Healthcare, Proton International London is proud to be able to offer PBT privately to adults and children from the UK and abroad, in London.
In Summary
Proton beam therapy is considered a good treatment option for certain types of skull base cancers for several reasons:
- Precise targeting: Proton beams can be precisely aimed and controlled to deliver radiation to a tumour while sparing surrounding healthy tissue, which is important for skull base tumours that are located near critical structures.
- Reduced side effects: By sparing healthy tissue, PBT can potentially reduce the risk of side effects and improve outcomes for patients.
- High dose delivery: Proton beams can deliver a high dose of radiation to the tumour, which can be particularly effective for certain types of skull base tumours that are resistant to other treatments.
- Favourable outcomes: Early studies suggest that PBT can result in high rates of tumour control and fewer side effects for certain types of skull base tumours.